Trends in Fitness to Practise: we are seeing fewer concerns and closing more cases at the early stages of the process
No one wants to be the subject of a fitness to practise investigation. It’s a stressful situation for any healthcare professional and can be both concerning and frustrating if the issues raised are felt to be minor and are ultimately resolved with no case to answer.
It is sometimes suggested to us that the GDC inflates concerns out of all proportion to their seriousness, often progressing cases all the way to a hearing when they could be resolved earlier.
We recognise that this, and similar views, may lead to unnecessary stress and unintended consequences as professionals report that they are practising defensively. To protect themselves, they’re spending considerable time explaining all possible treatment options to their patients while taking copious notes to describe what they said and did and doing it in considerable detail – time that could be better spent treating and caring for patients.
We want to explain how fitness to practise is changing. We are seeing signs that efforts to improve complaint handling through local resolution are having an impact, and some of our more recent process improvements are starting to have an effect. The initial inquiries pilot has the potential to improve things further.
We exist to protect the public. We are not out to get professionals, but we are told that it can feel that way when an investigation is underway. We need to do more to support individuals, but we also need to start tackling some of the long held but increasingly outdated beliefs that persist around fitness to practise, not least because they can have real world effects.
We are seeing far fewer concerns than a decade ago
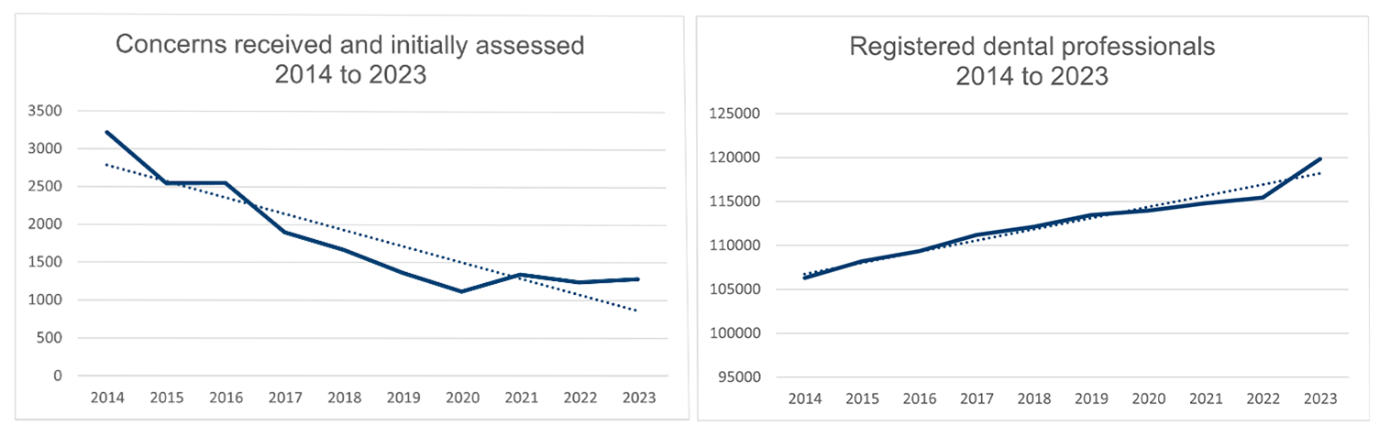
The number of concerns received and initially assessed has reduced by more than half over the last decade. Public confidence in the profession remains high. Over the same period, the number of people registered to practise dentistry in the UK has increased. What is behind this clear trend?
Work across the sector to emphasise the importance of good complaint handling has certainly contributed. The Dental Complaints Service has grown, helping to resolve issues raised in private practice, while reducing the number of issues they refer to us for an investigation. We have also seen new protections for whistleblowers and the introduction of the professional duty of candour.
Considerable effort has gone into ensuring that people can find guidance on how to provide feedback or make a complaint before raising it with us, and further improvements have been made in recent months. We have also updated our processes to help make sure people are directed to the organisation best placed to resolve their issues.
The majority of cases are resolved early in the process
Our strategic priority is to ensure that concerns are addressed effectively and proportionately to protect the public. While our legislation has been constraining, progress has been made.
When we receive a concern, we will make an initial assessment. That assessment will be based solely on the information we receive from the person who raised the concern. We have no further information to inform decisions at this stage. We must make further inquiries where the answer is yes to one or both of the following:
- harm has been or may be caused to a member of the public
- public confidence in the profession has been or may be undermined.
This low threshold means we need to open a case for the majority of concerns received. Typically, around 85% of all concerns considered by our Initial Assessment team are progressed for an investigation and proceed to the assessment stage. To be able to make an assessment, we need to gather more information, including contacting the registrant to request relevant records.
Last year, almost 40% of all cases opened for an investigation fell into the category of clinical complaints raised by a single patient. In terms of seriousness, these are generally at the lower end of the scale. Our initial inquiries pilot is focusing on these types of cases to see how we can resolve them at an earlier stage. We have recently announced that we are extending the pilot and, if we get the approach right, it has the potential to deliver significant benefits, including:
- reducing the impact of investigations on everyone involved
- earlier outcomes and opportunities to reflect on the issues raised
- freeing up resources to improve overall case progression and timeliness.
We have already noticed some positive impacts, with only 12% of cases assessed through the pilot being progressed to case examiners. The Assessment team has reported faster responses to requests for records. Our ability to make fully informed decisions quicker and earlier in the process depends on the cooperation of dental professionals, so we are grateful for the response we have received to our requests for records in the pilot’s first six months.
Record keeping is important to ensure high standards of care and can be helpful if things do not go to plan, but we do not expect anyone in the dental team to be creating unnecessary records. That is not what we or your patients expect. We are asking for complete and accurate records that are readable and taken at the time.
Clinical advisers will review records in these cases. They are asked to determine if your records demonstrate that the standard of care delivered has met the level of professional practice reasonably expected of someone working within that discipline. Shamir Mehta, Senior Clinical Dental Adviser, explains more in his blogpost, including what is professional, reasonable and in the interests of patients.
Our more recent efforts to conclude cases at an earlier stage builds on progress made as a result of reforms to legislation in 2016. The legislative changes made introduced case examiners, who were empowered to make outcome decisions in fitness to practise cases. Case examiners can:
- close a case
- issue advice or a warning
- ask a dental professional to agree to undertakings.
The change meant that cases, particularly the less serious ones, could be resolved earlier in the process without convening a panel and the parties having to attend a hearing. Clinical dental advisers were also brought into the GDC in 2016 to improve consistency in advice in clinical cases before being passed to case examiners for an outcome decision.
These changes had an impact - the number of cases progressed to a hearing fell by a third in a single year to a little over 200 cases. The number of cases referred to a hearing has stayed around this level over more recent years, but did fall to its lowest level in a decade last year.
Starting to see green shoots of further improvement
We say this a lot, but the number of concerns raised with us each year is small. The number of cases referred to the Dental Professionals Hearings Service for a hearing is even smaller against a backdrop of a growing number of people working in dentistry as part of the dental team.
In 2016, 333 cases were referred for a hearing, representing about three registrants in every 1,000 (0.3%) on the register that year. Seven years later in 2023, we referred just 132 cases, or around one registrant in every 1,000 (0.11%). While the total number of cases being progressed to a hearing has remained quite static over more recent years (ranging between 132 to 176 cases over the last four years), increases in the number of professionals on the register means that the proportion of cases progressed to a hearing has reduced.
The impact of changes made over several years is now being reflected in the figures and performance. We have made a number of improvements over the past two years, including increasing our staffing in 2022 to help to ease pressure on existing colleagues, and our staff retention rates have improved. The position is shifting and, as a result, in April and May we managed to outperform our targets for cases to reach an Assessment decision for all case types.
We are currently processing an active caseload at assessment of around 550 cases.
The reality of fitness to practise is that the number of serious concerns raised has reduced significantly over recent years and we are progressing fewer cases to the later stages. We have more to do to improve timeliness and the support provided to individuals, but the indications are that efforts across the sector to improve complaint handling and reduce the impact of investigations are having an effect and we are moving in the right direction.
Find out more about fitness to practise
We recently published the 2023 statistical report for fitness to practise, which provides the case numbers and details about the types of concerns raised with us.
You will also find a detailed analysis of our case file data in recently published research from the University of Plymouth, Unlocking the potential of GDC fitness to practise data.
We provide information and contact details for organisations that can help if you need support.
You will find more guidance on record keeping in our next post by Shamir Mehta, Senior Clinical Dental Adviser.
 eGDC
eGDC











